As the number of conditions treated with botulinum toxin (BTX) increases, so does the importance of clinicians understanding the intricacies of billing and coding for this therapeutic agent. Unfortunately, even after a clinician feels comfortable with neurotoxin injection technique, the process of authorization, billing, and coding may still seem daunting. Clinicians need to be familiar with the purchase and storage of BTX, prior authorization requirements across insurers, and appropriate documentation of indications and procedures. Correct coding, using current procedural terminology (CPT) and International Statistical Classification of Diseases, 10th revision (ICD-10), linkage is critical for successful integration of BTX therapy into clinical practice (Box 1).1
BOX 1. Tips For Initiating Therapy With Botulinum Toxin
- Ensure proper documentation justifying:
- need for botulinum toxin (BTX),
- prior treatment failures, and
- injection plan.
- Prepare a letter of medical necessity that includes:
- preferred toxin,
- ICD-10 diagnosis codes,
- prior treatment failures,
- requested number of vials,
- CPT procedure codes, and
- guidance procedure code.
- Schedule patients with traditional Medicare/Medicaid as soon as possible because prior authorization is not required.
- Schedule those with private insurance or a Medicare/ Medicaid health maintenance organization (HMO) plan in approximately 3 to 4 weeks to:
- verify benefits and obtain prior authorization;
- receive BTX from a specialty pharmacy if required; and
- avoid multiple calls from patients inquiring about status.
- Obtain consent at time of scheduling from patients with private insurance or Medicare/Medicaid HMO if a prior authorization service may be utilized.
Prior Authorization
Medicare, Medicaid, and private insurances cover BTX treatment for on- and off-label uses considered medically necessary. Uses for many off-label conditions (eg, oromandibular dystonia or limb dystonia) are considered standard of care and are commonly approved. Medicare policies can vary from state to state, but private insurance policies are typically universal. Being familiar with the policies in your state can save time and frustration when submitting prior authorization.
With traditional Medicare or Medicaid, no prior authorization is needed for BTX. Payment will occur if the procedure is covered by your state’s policy and if the proper linkage between ICD-10 code and CPT code is documented. Prior authorization for BTX, including for on-label uses, should be obtained for all patients with private insurances or Medicaid/Medicare health maintenance organization (HMO) and Medicare/Medicaid. Prior authorization can be requested by contacting the insurance company directly or by using the BTX manufacturer’s prior authorization services, which can expedite approvals and save staff time. Patients must give written consent to allow the company to contact their insurance provider. An office note justifying the reasoning for BTX treatment and discussing failed treatment along with a letter of medical necessity should always be included with the prior authorization request (Box 1).
Benefit verification is first performed to ensure the patient’s insurance policy is current and covers injectable treatments such as BTX. Benefit verification does not equal preapproval or medical necessity. Prior authorization must be performed to increase the probability of proper payment. Most insurance companies will grant prior authorization for 6 to 12 months or for 2 to 4 treatments. Injections need to be performed within this authorization window or payment could be denied. Authorization results typically include approved dates of service and approved CPT codes. The allowable number of toxin units and how to obtain the drug (ie, the buy-and-bill process vs using a specialty pharmacy) are also reported.
Ordering, Storing, and Billing for BTX
BTX procurement options include buy-and-bill by the practice or provided by a specialty pharmacy. Traditional Medicare and some private insurance companies require practices buy-and-bill the drug. Many private insurers require the use of a third-party specialty pharmacy. The use of a specialty pharmacy may limit risk of lost funds from insurance denials; however, it also reduces total reimbursem*nt. If clinicians obtain BTX and bill from their stock, a margin above the cost of the drug is reimbursed. For Medicare, the margin is up to 6% above the average wholesale cost, making buy and bill minimally profitable. Margins for private carriers or workers’ compensation benefits may be much larger, making buying and billing more attractive. Your billing staff should be able to provide an expected margin per unit for each major insurance carrier. OnabotulinumtoxinA (Botox; Allergan, Madison, NJ) and incobotulinumtoxinA (Xeomin; Merz, Raleigh, NC) are billed by the single unit, abobotulinumtoxinA (Dysport; Ipsen, Cambridge, MA) per 5 units, and rimabotulinumtoxinB (Myobloc; Supernus, Rockville, MD) per 100 units. Remember that both the amount of drug used for injection and the drug wasted should be charged. For example, if a 200-unit vial of onabotulinumtoxinA is mixed to inject a person being treated for chronic migraine with 155 units, the 45 units wasted are also billed. When billing waste, add a JW modifier (Table 1).

Click to view larger
Availability of toxin samples, discounts, and patient assistant programs varies among companies. Check with your local BTX manufacturer’s representative for such programs. Each toxin can be ordered directly from the manufacturer with expected next day arrival. Avoid placing orders that could arrive on the weekend for toxins that require refrigeration. It is recommended that all of the toxins be stored together in a locked refrigerator between 2°C and 8°C with a temperature alarm. In the case of specialty pharmacies, have the drug sent directly to your office rather than the patient’s home to ensure proper storage. A separate log for drugs obtained by the practice and another for drugs obtained from specialty pharmacies is recommended, with documentation of lot numbers. Regular reconciliation of inventory on a weekly or monthly basis is also suggested.
Procedure Coding, Documentation, and Billing
Proper documentation is essential for correct payments (Box 2). A procedure note should be detailed and include diagnosis, site, injection location, dilution, electrophysiologic/ultrasound guidance, provider of medication (buy-and-bill vs specialty pharmacy), amount of BTX used, amount wasted, approval dates, and prior authorization number. Although not essential, insurance companies like to see a written procedure note with a diagram of the areas injected and an outline of the specific dosages injected at each site. From a clinical perspective, this makes reproducing injections in the future easier. For ongoing treatment, response to therapy should also be clearly documented. A real-time inventory log is suggested with the date of service, amount, and source of BTX (practice stock vs specialty pharmacy), along with the patient’s name/medical record number, and lot number in case of an unexpected side effect or drug recall. This can be performed using an inventory management system or by creating a spreadsheet.
BOX 2. Botulinum Toxin Billing And Coding Pearls
- Be aware of which insurance carriers in your area allow for injections to be performed every 12 weeks (84 days) vs every 90 days or 13 weeks, to ensure payment.
- Medicare requires the proper CPT code linked with the approved ICD-10 code for reimbursem*nt.
- Medicare may not pay for buy-and-bill of the toxin if the patient is in a nursing home.
- Store all toxins in a locked refrigerator, remembering to:
- record temperature daily and
- link the thermostat to your alarm system to prevent loss of the drug in case of faulty refrigerator or power outage.
- Keep separate inventory logs of stock drug with lot number, date received/injected, and whether from buy-and-bill or specialty pharmacy.
- Consider collecting the patient’s expected coinsurance amount before scheduled injection, similar to what is commonly done for surgical procedures.
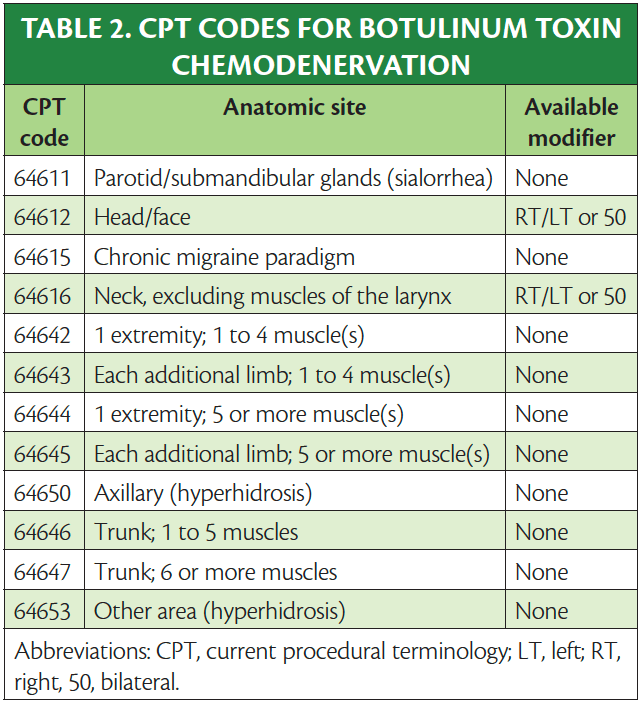
CPT Codes for Chemodenervation
Specific chemodenervation codes for BTX are based on the appropriate anatomic location site injected (Table 2).2-5 The Centers for Medicare and Medicaid Services (CMS) will allow payment for 1 injection per site, regardless of the number of injections made into the site.6 For injection into bilateral parotid and/or submandibular glands for sialorrhea use CPT 64611 only once with no modifier. Any injection in the cranium (64612) including corrugator, frontalis, temporalis, occipitalis, facial muscles, and masseter are considered head/face. This code can be used bilaterally using the right (RT), left (LT), or bilateral (50) modifiers. All injections within the chronic migraine paradigm are considered 1 site (64515) even though injections are performed in the head/face, cervical paraspinals, and trapezii, and no modifiers are permitted.
Both axillae are considered 1 site (64640 chemodenervation of eccrine glands) and can only be used once per session. When injecting for hyperhidrosis in other sites (eg, scalp, face, or extremities), use 64643, chemodenervation of eccrine glands; other area(s). For injections of neck muscles for conditions (eg, cervical dystonia) use code 64616 (chemodenervation of neck muscle(s) excluding muscles of the larynx), which can be used bilaterally using RT, LT, or 50 modifiers.
Chemodenervation of 1 or more extremities involves the use of several different CPT codes. The first code is known as the base code and should represent the limb with the most muscles injected. Pick code 64642 chemodenervation of 1 extremity; 1 to 4 muscle(s) or 64644 chemodenervation of 1 extremity; 5 or more muscle(s). Further limb injections can be billed using add-on codes based on the number of muscles injected in each limb. No modifiers are necessary. For each additional extremity, 1 to 4 muscle(s) injected, use +64643 and for each additional limb injected, 5 or more muscles, use +64645.
Trunk muscles are an independent region that includes the erector spinae/paraspinal muscles and rectus abdominis/obliques. Use CPT code 64646 when injecting 1 to 5 muscles and 64647 for 6 or more. Each code can only be used once per session. Based on the site definition above, muscles such as the trapezius/levator scapulae (below C7), rhomboid, gluteus, and piriformis are considered limb/limb girdle muscles.
Modifiers
Insurance companies allow the addition of modifiers RT, LT, or 50. Check with your local carriers to determine when to bill with a modifier and which modifier is appropriate (Table 3). Typically, if a code is listed a second time on the billing sheet without a modifier, it is automatically kicked out as a duplicate. Some codes such as 64611 and 64615 can be used only once per injection session and, therefore, modifiers will not apply.
The use of an evaluation and management (E/M) code along with a BTX procedure is discouraged. This coding is only appropriate if a separate identifiable medical service is provided for a different diagnosis than the one used for BTX. For example, if a patient with Parkinson disease (PD) is seen for medical management of PD and also receives treatment with BTX for sialorrhea, an E/M could be used with a -25 modifier. It is imperative that the medical diagnosis is linked to the E/M and that the other diagnosis (in this case sialorrhea) is linked to the CPT code to ensure proper reimbursem*nt.
Anatomic Guidance
To ensure efficacy and safety, electrophysiologic or visual guidance is suggested for many injection locations. Electromyography, muscle stimulation, and ultrasound can be used independently or together based on clinical necessity. Medicare, for instance, allows for electromyography or electric stimulation to be performed with ultrasound guidance. Use of these techniques maximizes clinical efficacy, decreases potential side effects, and is reimbursable. Table 4 reviews the CPT codes for BTX injections under anatomic guidance. Each code can be used once per date of service.
Reimbursem*nt and Collections
Be familiar with your major regional insurance policies for BTX to help reduce delays in payment and even denials. Review each claim before the patient’s next injection cycle to ensure the procedure, anatomic guidance, and drug have all been paid in accordance with your payer contract. Commonly, the carrier may only pay for procedures that are considered medically necessary. If a particular code is paid bilaterally by a payer, reimbursem*nt for the second side is typically reduced by half. Each toxin company has reimbursem*nt specialists that can assist in billing and coding, insurance verification, local coverage policy support, and claims denials and appeals. Consider requesting an analysis every 6 to 12 months to avoid loss of revenue and repetitive billing errors.
1. American Medical Association. CPT Standard - Current Procedural Terminology (Standard Edition). 1st ed. American Medical Association; 2013.
2. Botox. Prescribing information. Allergan Inc; 2021.
3. Dysport. Prescribing information. Ipsen Biopharm Ltd; 2020.
4. Myobloc. Prescribing information. Solstice Neurosciences, LLC; 2019.
5. Xeomin. Prescribing information. Merz Pharmaceuticals, LLC; 2021.
6. Centers for Medicaid & Medicare Service. 2022 ASP Drug Pricing Files. Updated March 9, 2022. Accessed March 14, 2022. https://www.cms.gov/medicare/medicare-part-b-drug-average-sales-price/2022-asp-drug-pricing-files
MT is on the speaker’s bureau and serves as a consultant to Abbvie and Biohaven and has received grants from Abbvie, Neurocrine, Ipsen, and Aeon
LB is on the speaker’s bureau and serves as a consultant to Abbvie, Acadia, Acorda, Amneal, Ipsen, Jazz, Kyowa Kirin, Neurocrine, Sunovion, Supernus, and Teva
CD is a consultant for Abbvie, Biohaven, Impel, Eli Lilly, Lundbeck, Novartis, Theranica, and Regeneron and has received clinical trial grants from Abbvie, Eli Lilly, Amgen, and Axsome